Food Safety
·
Wash Your Hands! Whenever you are preparing
food, it is so important to wash your hands before, during and after to prevent
food poisoning. (And spreading germs!)
·
Always make sure to cook food well to reduce
potential poisoning- poultry-180 degrees F, beef-160 degrees F and pork-160
degrees F. Cover and reheat leftovers to
165 degrees Fahrenheit before serving.
·
Keep cold foods cold and hot foods hot.. If food
is left out at room temperature for more than two hours, bacteria can grow and
sickness can ensue. This means leftovers should be put up right away.
·
Never use unvented fuel-burning devices in a
home or apartment, because carbon monoxide (CO) poisoning can occur. Read our
blog on CO poison safety here.
·
Remember, contaminated food is not always evident.
If you are unsure if an item is still okay to eat, it is probably best to throw
it out. Safety first!
Potentially Dangerous
Décor
Tree Ornaments:
Some ornaments are made of very thin metal or glass. If a child were to ingest
part of an ornament, it could potentially cause them to choke. Practice safety
first when choosing ornaments to use on your tree with little ones in the home.
You can find lots of ornaments offered in stores that are unbreakable and best
to use around children.
Gift Wrap:
Overall, gift wrapping paper is pretty safe. But it is possible for some
colored gift wrap or foil to contain lead. Don’t let babies chew on paper as a
precaution.
Holiday Plants
Poinsettia: The
poinsettia’s reputation is worse than it merits. In reality, the poinsettia is
a minimally poisonous plant. If ingested in very large amounts it may cause
varying degrees of irritation to the mouth, nausea or vomiting. The sap on the
plant can also cause a skin rash, so when handling these plants, make sure to
wash your hands with soap and water afterwards as a precaution.
Holly berries:
While these berries are visually appealing, if ingested they can cause a
stomach ache, nausea, vomiting and diarrhea. Keep these berries out of reach of
children.
Mistletoe: If this
plant is ingested, it can leave you feeling a little crummy. Common symptoms of
ingestion can include vomiting, diarrhea and stomach ache.
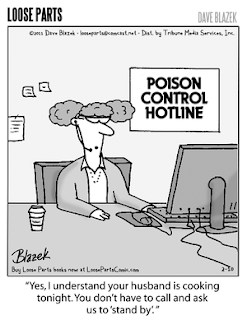
Remember, as always, if you or someone you know is
potentially poisoned, please do not hesitate to contact the Poison Control
hotline at 1-800-222-1222. We hope everyone has a safe holiday season!